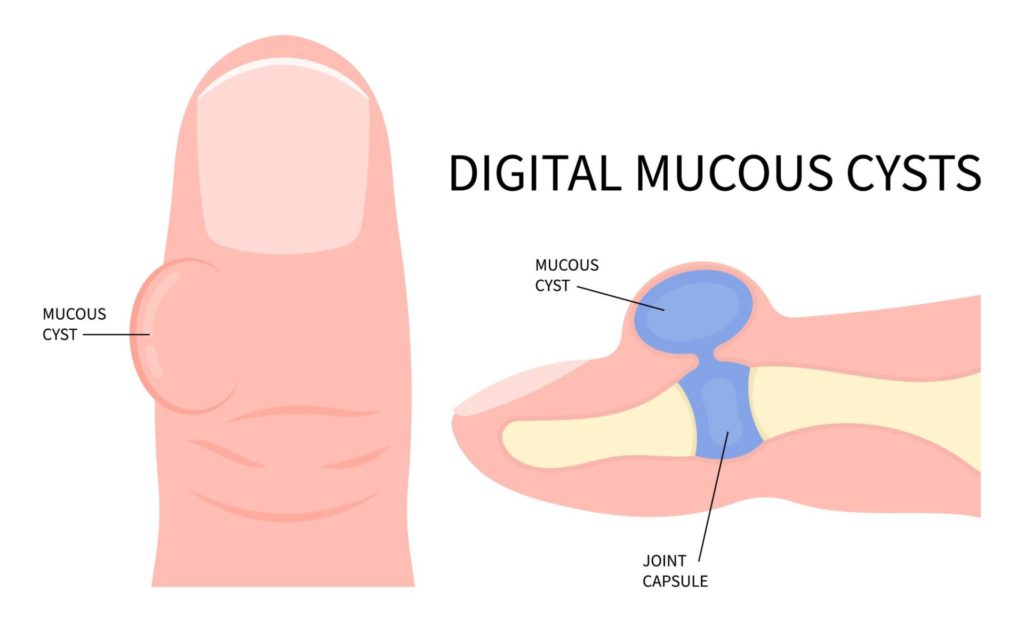
Digital mucous cysts, also referred to as myxoid cysts, are small, shiny growths that typically develop near the nail bed on the fingers or toes. Described as a type of ganglion cyst, these growths are often linked to underlying conditions like osteoarthritis.
In this blog, we’ll explore the main causes of digital mucous cysts, the symptoms to watch for, and the treatment options available to help manage them.
Who do they affect?
Although digital mucous cysts can affect people of any age, they are most commonly seen in adults over the age of 40. Women in this age group are three times more likely to develop these cysts than men.
This increased prevalence in women may be related to hormonal changes or a higher incidence of osteoarthritis, a condition strongly linked to the formation of mucous cysts. Studies show that between 64% and 93% of individuals with osteoarthritis also develop digital mucous cysts.
Causes
Osteoarthritis
As mentioned earlier, osteoarthritis is the leading cause of digital mucous cysts due to the way it affects your joints over time. When you have osteoarthritis, the cartilage that cushions the ends of your bones starts to break down. As the cartilage wears away, the bones begin to rub against each other, which leads to inflammation and joint damage.
The joints can become less stable as osteoarthritis progresses, and the soft tissues around them weaken. This breakdown creates space for fluid to collect, which can form a cyst. In the case of a digital mucous cyst, the synovial fluid, normally responsible for lubricating your joints, can leak out and accumulate just under the skin, typically near the nail bed, resulting in a cyst forming.
Osteoarthritis also often causes inflammation and increases pressure within the joint, which can push that synovial fluid out of the joint capsule, prompting a cyst. Essentially, the cyst is an outpouching of the joint capsule or tendon sheath filled with this thick fluid.
As your osteoarthritis progresses, it also changes the surrounding tissues like ligaments and tendons. These tissues become more prone to forming cyst-like structures, such as digital mucous cysts. In a way, these cysts are your body’s response to the constant irritation and inflammation caused by the underlying arthritis.
In the later stages of osteoarthritis, bone spurs (or osteophytes) can develop around the affected joints. These spurs can further irritate the surrounding tissues, increasing the likelihood of cyst formation as your body reacts to the ongoing damage.
Focal Mucinosis
Focal mucinosis occurs when there’s an unusual accumulation of mucins, which are gel-like proteins found in the body’s connective tissue. Normally, mucins help keep tissues lubricated, but in this condition, they build up excessively beneath the skin, particularly around the fingers or toes. This accumulation leads to the formation of a cyst, often appearing as a smooth, translucent bump near the nail bed.
Unlike cysts caused by joint degeneration, focal mucinosis is not linked to arthritis or other joint-related issues. Instead, it’s thought to be related to changes in the skin’s connective tissue.
In focal mucinosis, the fibroblasts (cells responsible for producing connective tissue) start producing too much mucin. This overproduction can create small pockets of fluid-filled tissue, which eventually form a cyst.
Because focal mucinosis isn’t driven by joint damage, the cysts that develop tend to be softer and less associated with pain or stiffness than those caused by osteoarthritis. They may feel more superficial and not as deeply connected to the underlying structures like tendons or bones. While they can be a cosmetic concern or cause discomfort due to their location, they aren’t typically linked to more serious underlying conditions.
It’s important to note that focal mucinosis is relatively rare, and these cysts can often appear without warning or a clear trigger. However, their development could be tied to minor skin trauma, repetitive stress, or even hormonal influences, although these connections are less understood.
Symptoms
Digital mucous cysts are typically small, measuring less than 1 cm in size. They can appear in various shades, from skin-coloured to slightly red or even translucent, and often have a dome-shaped appearance.
In most cases, you’ll find them at the base of the nail bed, and they’re most likely to show up on the index or middle finger of your dominant hand.
Sometimes, these cysts can form just beneath the nail, leading to discolouration at the base, which may look like a darker spot or streak. Occasionally, they can leak a clear, sticky fluid, or even fluid tinged with blood. Usually, only one cyst develops at a time, but in some cases, you might find more than one on the same finger or hand.
While they might be small, these cysts can still cause discomfort, especially if they affect nail growth or become irritated.
Treatments
Surgical Removal
Surgery is the most effective treatment, with a success rate of over 90%. During the procedure, the surgeon will remove the cyst entirely, and in some cases, they may inject a dye into the joint to locate and seal the source of the fluid leakage. This prevents the cyst from reoccurring, addressing the root cause.
Non-Surgical Options
If you prefer to avoid surgery, there are non-surgical methods available, though they may require multiple treatments to be fully effective.
- Sterile Draining
One common approach is to have the cyst drained using a sterile needle or blade to puncture it. This allows the fluid to be released, reducing the size of the cyst. However, because the cyst can fill back up, this procedure may need to be repeated 2 to 5 times to achieve long-term results. - Steroid Injections
Steroid injections can be used to shrink the cyst by reducing inflammation and fluid production. This option can be effective, but it may not prevent the cyst from returning over time. - Cryotherapy
Cryotherapy involves draining the cyst and then applying liquid nitrogen to freeze and thaw the area. The freezing process blocks the flow of fluid to the cyst, reducing the chance of recurrence. This method is less invasive than surgery but may also require follow-up treatments.
Each treatment option has its benefits, and your doctor can help you decide which is best for your specific case. Surgery offers the highest success rate, but non-surgical methods are good alternatives if you’re looking for less invasive approaches.
If you have further queries or would like to find out more information about your condition, get in touch with us today.