This is a genetic condition and is not a serious or life-threatening problem. It is usually painless but can interfere with certain functions of the hand. However, treatment is not always indicated and is offered if the condition is progressing rapidly or causing you significant functional problems.

Dupuytren’s Disease Treatment
Book Appointment
Causes of Dupuytren’s Disease
The condition starts with the appearance of a lump or band in the palm of your hand, developing over a period of time. This lump is usually painless but can be tender when it is rapidly growing or on direct pressure. Over time the lump can develop into a band passing into the fingers leading to the finger contracture. When a contracture is developed fingers do not straighten up and you can get problems putting your hand in a pocket or putting on gloves.
This tissue is similar to the scar tissue and becomes a problem when fingers can not straighten. This has no relation to finger tendons.
The condition can occur in other parts of the body and is known by other names:
- Soles of feet: Plantar fasciitis.
- Penis: Peyronies disease.
- Over the knuckles: Garrod’s pads.
Risk factors of Dupuytren’s Disease
The commonest cause is genetic where it is inherited from one of your parents or grandparents, however, other factors can increase the risk or severity of the disease:
- Alcohol abuse.
- Smoking.
- Epilepsy medication.
- Injury to the hand
- Diabetes.
Conservative Treatment with Splint
There is some evidence that splints worn at night time (to keep the fingers straight) will help to prevent disease progression, however, the success rate of treating the condition is very low and will not be helpful in rapidly advancing disease.
Injections
Steroid injections into the painful lump in the palm have a 50% success rate in improving the symptoms however this is short-lived, does not prevent the disease progression and is a very painful procedure.

Surgery for Dupuytren’s Disease
Different types of surgery treatments are indicated depending on the different stages of this Dupuytren’s disease.
Needle aponeurotomy
This is the simplest form of treatment where under local anaesthetic the cords in the palm are released with a needle and allow the fingers to straighten up. This is indicated if the disease is only in the palm.
Segmental fasciectomy
This is usually reserved for more extensive disease in the palm and sometimes in the fingers. A section of the cord is excised under local anaesthetic as a day-case procedure. There will be a few stitches which need to be removed after 10-14 days.
Fasciectomy
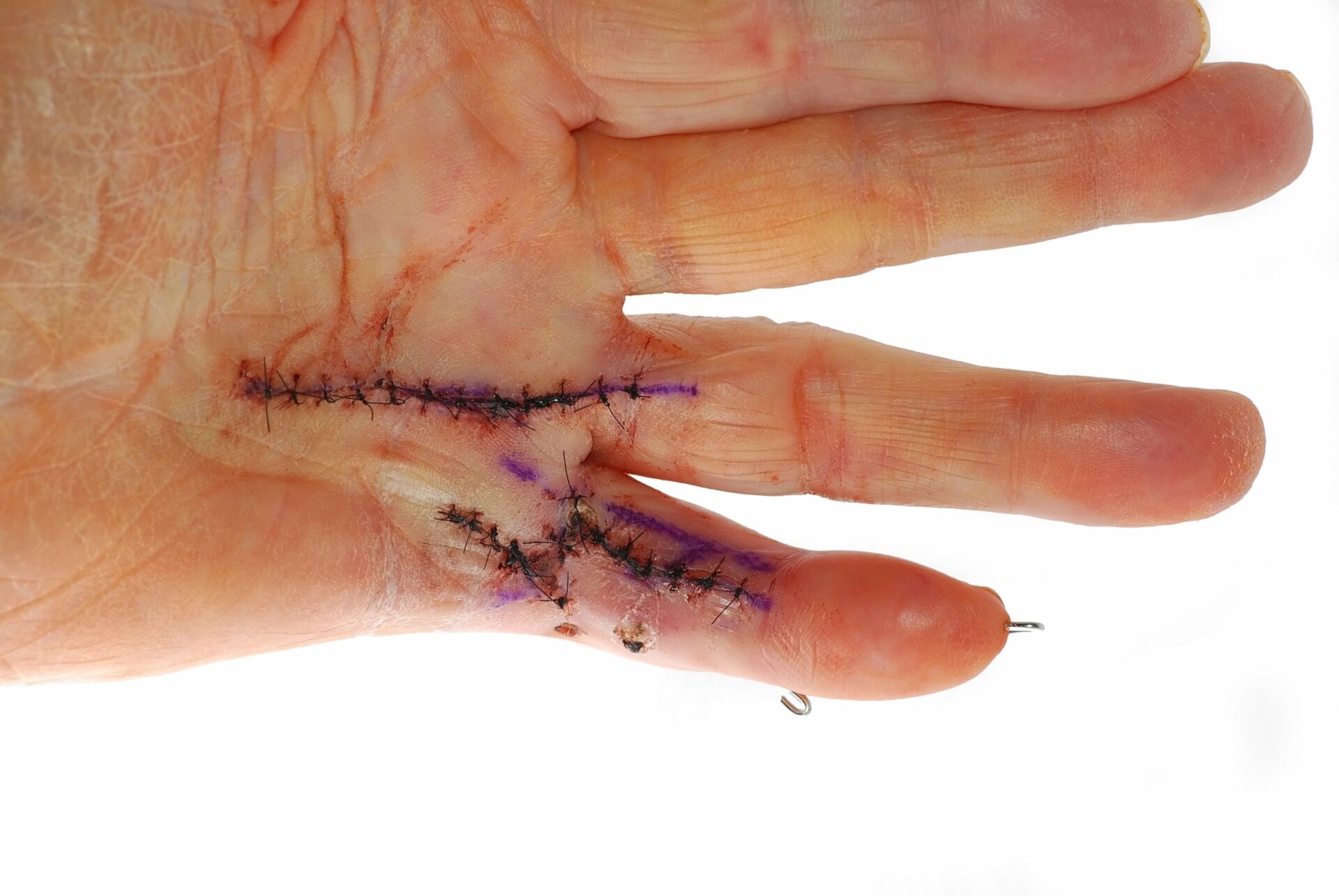
This is the most common operation for Dupuytren’s Contracture where the disease has extended deeply into the finger. This operation can be done under a general anaesthetic (you will be asleep) or regional anaesthesia (you will be awake but the operated hand is anaesthetised). During this operation, the diseased area under the skin is removed as much as it is safely possible. Zig-zag incisions are used to reduce the risk of recurrence.
Dermofasciectomy
In very severe or advanced diseases the skin overlying the diseased finger is also involved or damaged as a result of previous surgery and therefore needs to be removed during the revision procedure. The area where the skin has been removed is covered by a skin graft (usually taken from the same arm).
Repeat operations
Revision surgery is usually carried out for severe recurrence of the disease following the initial surgery. This is a longer and more extensive procedure that requires surgery on the affected joints. A skin graft may be necessary as the diseased skin following the recurrence is removed.
Joint fusion or amputation
These procedures are rare and considered the last stage of operation. They are reserved for severe joint contracture and previously operated fingers with severe recurrence of finger contracture.
Aftercare and Follow Up
Dressings
You will have a big bandage and Plaster of Paris on your hand which will be changed between 7-10 days from the time of surgery. You will be seen in the clinic 7-10 days after your surgery for a wound check, change of dressings and application of a night splint which is made by a hand therapist. The stitches are usually removed after approximately 2 weeks. Some wounds and skin grafts require longer periods of dressing.
Hand Therapy
During the surgery, the fingers have been corrected from a bent to a straight position. Physiotherapy will be necessary to help you move the fingers after surgery which can be quite painful and may be necessary for up to 6 months.
Splints
Night splints are used to keep the fingers straight at night time when they are usually curled in during sleep. They are meant to reduce the risk of recurrence and I recommend them to be worn for at least 6 months or longer if possible.

Risks of Surgery
Incomplete correction
It may not be possible to fully straighten the finger if it has been bent for many years, or if the finger is bent at the small joints, or if there is arthritis within the affected joints as a result of prolonged joint contracture.
Nerve damage
The Dupuytren’s tissue is always wrapped around the small nerves and blood vessels in the finger. There is a risk of nerve damage (5-10%) while the diseased tissues are removed, despite using magnification loops during the procedure. Nerve damage can lead to some permanent or temporary loss of feeling at the tip of the finger.
Scar pain and Cold sensitivity
Up to 10% of patients experience cold sensitivity after surgery to fingers which responds well to keeping the fingers warm in wintertime. Scar sensitivity usually improves with scar desensitisation exercises provided by the hand therapist.
Recurrence
As this is a genetic condition there is a risk of recurrence after surgery, however majority of patients do not require any surgery. The risk of recurrence is higher after surgery on the little finger (15%).

Infection
There is a small risk of infection (<1%) after surgery. Patients with diabetes and those with urinary tract or chest infections close to the time of surgery are at higher risk of developing infection after surgery. This may lead to further surgery and possible amputation if the infection is severe or uncontrolled.
Skin graft failure
10% of skin grafts can fail partially or completely and therefore prolonged dressings or a further skin graft may be necessary.
Joint pain and stiffness
Small joints of the fingers are very sensitive to surgery and can become stiff after surgery which can lead to reduced movement of the finger. Physiotherapy usually helps with improving joint stiffness however in some patients this can be persistent.
Reflex sympathetic dystrophy
This is a rare condition that affects patients who have had an injury or surgery to the hand. It is diagnosed by the presence of severe pain, swelling and stiffness in the hand which may persist for up to 2 years. Patients require extensive physiotherapy and pain medication.
Book an appointment
Please use this form if you are interested in booking an appointment. We do not give general medical advice over email.